Super User
Why Walking in High Heels Can Be Challenging

High heels are undoubtedly stylish and add an elegant touch to any outfit, but there is no denying that walking in them can be a daunting task for many. Several things make it difficult to walk gracefully and comfortably in high heels. First, the angle of the foot in high heels forces the wearer to put most of their body weight on the balls of the feet. This shift in weight distribution can lead to instability, causing a precarious and unsteady gait. Second, the elevation of the heel shortens the Achilles tendon and calf muscles, making it challenging to take regular, longer strides. This altered biomechanics can cause discomfort and make walking feel unnatural. Additionally, the pressure and friction created by the narrow, pointed shape of high heels can lead to blisters, calluses, and foot pain. In essence, the difficulty of walking in high heels is not merely a matter of fashion; it is a matter of biomechanics and comfort. For many, it is a skill that requires practice and endurance. So, while high heels can make a powerful fashion statement, they also pose a challenge for those who dare to wear them. If you would like more information on how high heels can affect the feet and better alternatives to consider, it is suggested that you speak with a podiatrist.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact one of our podiatrists from Florida Ankle & Foot Institute. Our doctors can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact our offices located in Tavernier, Marathon, and Key West, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Effect of High Heels on the Feet
High heels are uncomfortable, but many women sacrifice comfort to be stylish. There are many problems that stem from wearing high heels, however these issues can be avoided by wearing proper shoes.
Heels are bad because they push your weight forward toward the fall of the foot. The higher the heel is, the more weight and pressure get shifted. This process causes the back to hyperextend backwards to counterbalance which may cause pain in the leg, hip, and back. Consequently, major posture problems may occur, and these issues may eventually become permanent.
Wearing high heels is one of the leading cause of ingrown toenails. Heels create a great deal of pressure on the big toenails which disrupts proper toenail growth. This may eventually lead to the big toenail growing into the skin. Another common problem that stems from high heels is bunions. If bunions go untreated, they can cause serious scar tissue to form along with severe pain.
However, there are ways to minimize the harmful risks associated with wearing heels. You should try to massage and stretch your legs and feet after wearing heels for an extended time. Stretching helps prevent the Achilles tendons and calf muscles from becoming too tight. A good substitute for heels are platforms which provide a better surface area to evenly distribute the body’s weight.
If you are experiencing any painful foot conditions from wearing high heels, you should consult with your podiatrist right away.
Understanding the Condition Called Neuropathy

Neuropathy, often referred to as peripheral neuropathy, is a complex and often misunderstood medical condition that affects the peripheral nerves, which are responsible for transmitting signals from the brain and spinal cord to the rest of the body. This disorder disrupts the normal functioning of these nerves, leading to a range of symptoms. Neuropathy can manifest as tingling, burning, or stabbing sensations, often in the hands and feet, but it can affect other areas as well. Numbness, weakness, and muscle atrophy may occur over time. The condition can be caused by various factors, including diabetes, certain medications, and infections, in addition to genetic predispositions. Managing neuropathy involves addressing the underlying cause if known, and alleviating symptoms. Treatments may include medication to manage pain and lifestyle adjustments to prevent further nerve damage. Understanding neuropathy is the first step in seeking appropriate care and support for those affected by this challenging condition. If you are experiencing symptoms of neuropathy, it is suggested that you schedule an appointment with a podiatrist who can accurately diagnose and treat this condition.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with one of our podiatrists from Florida Ankle & Foot Institute. Our doctors will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Tavernier, Marathon, and Key West, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Trench Foot

Trench foot, also known as immersion foot syndrome, is a serious condition resulting from prolonged exposure of the feet to moisture. It damages the circulation and nerve function in the feet. Its history goes back to World War I when soldiers in cold, wet trenches suffered from it due to wearing inadequate footwear. The symptoms of trench foot include blisters, blotchy skin, redness, and possibly tissue loss. It can also cause sensations such as coldness, numbness, and persistent itching. Trench foot is primarily caused by wet feet that do not dry properly, with temperatures that are 30˚F to 40˚F being most conducive. Early treatment is essential, and, if left untreated, trench foot can lead to severe complications such as amputations, gangrene, and permanent nerve damage. Diagnosis involves a physical examination by a doctor to assess injuries, tissue loss, and circulation. Treatment mainly consists of rest, elevation, pain medications, and keeping the feet clean and dry. Prevention includes keeping feet dry, having spare socks and shoes on hand, and airing out feet after wearing socks and shoes, even if they do not appear wet. If you have sustained prolonged exposure of your feet to moisture and have symptoms that are worsening, it is strongly suggested that you make an appointment with a podiatrist as soon as possible for a proper diagnosis and treatment.
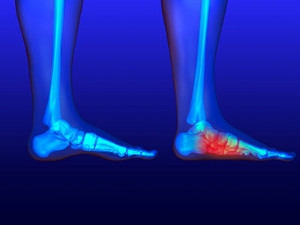
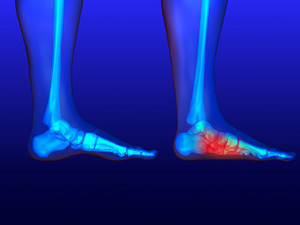
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Florida Ankle & Foot Institute. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Tavernier, Marathon, and Key West, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Running With Flat Feet
Running is a pursuit that empowers both body and mind, regardless of foot arch type. Flat feet, often misunderstood, should not deter anyone from lacing up and hitting the track. There are various types of flat feet, each requiring a unique approach. Flexible flat feet involve arches that appear when one is off the foot, and rigid flat feet exhibit little to no arch, even when lifted. While some flat feet do not pose issues, others may lead to discomfort or pain during running. Wearing customized footwear with proper arch support is essential. Orthotics or insoles can aid in maintaining alignment and reducing strain. Performing strengthening exercises targeting foot muscles can enhance stability. Running with flat feet is indeed possible with the right knowledge, care, and preparation. If you have flat feet and are interested in pursuing running as a hobby, it is suggested that you are under the care of a podiatrist who can provide you with useful information.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from Florida Ankle & Foot Institute. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Tavernier, Marathon, and Key West, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Flexible Flat Foot?
Flatfoot is classified as having the entire sole of the foot in contact or near contact to the ground while standing. The disorder is also known as fallen arches, because those affected have no arch in their feet. Flexible flatfoot and rigid flatfoot are the two types of flatfoot.
A person has flexible flatfoot if when sitting or standing on their toes, they have an arch that disappears when they stand with the entire foot on the ground. Flexible flatfoot may also be called “pediatric flatfoot” because the condition first appears in childhood. It is common among infants because the arch does not develop until the age of 5 or 6 years. Rigid flatfoot is not as common in children as it is with adults. This type of flatfoot is developed due to the weakening of tibialis posterior muscle tendon, a major supporting structure of the foot arch. Development of this deformity is progressive and shows early signs of pain and swelling that begins at the inside arch of the foot and moves to the outside of the foot below the ankle. More severe cases can possibly lead to arthritis of the foot and ankle joints.
Although most cases of flatfoot involve people born with the condition, some less common causes are obesity, diabetes, pregnancy, and osteoporosis. In some cases, flatfoot may come with no symptoms at all and does not require any type of treatment. With other cases though, symptoms may include pain in the shin, knee, hips and lower back. If a person with flatfeet experiences such symptoms, a health care provider may suggest using orthotic devices or arch supports, which may reduce the pain. Wearing supportive shoes can also prove more comfortable with flatfeet and staying away from shoes with little support such as sandals. Other methods to relieve pain also include stretching the Achilles tendon properly and using proper form when doing any physical activity. In addition, losing weight can reduce the stress on your feet and reduce the pain.
How Rheumatoid Arthritis Affects the Feet

Rheumatoid arthritis, abbreviated RA, is a relentless autoimmune disorder that does not spare the feet from pain. The immune system's misguided attacks on the synovium, which is the protective lining of joints, lead to chronic inflammation in various parts of the body, including the feet. The small joints in the toes, the arch, and the ankle are frequent targets, causing swelling, stiffness, and pain. Over time, RA can lead to deformities, such as bunions, hammertoes, and collapsed arches, resulting in altered foot structure and gait. The chronic pain can impair mobility, leading to a reduced quality of life. Early diagnosis and prompt intervention are crucial to managing symptoms and slowing down the progression. A treatment approach involving medication, wearing orthotics, and incorporating lifestyle adjustments may help to alleviate the burden on the feet and enhance overall foot health for individuals with RA. If you have this condition, it is strongly suggested that you are under the care of a podiatrist who can offer you additional relief options.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact one of our podiatrists of Florida Ankle & Foot Institute. Our doctors will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our offices located in Tavernier, Marathon, and Key West, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Rheumatoid Arthritis is a chronic progressive disease that attacks several joints throughout the body. It is an autoimmune disease in which the body’s immune system mistakenly attacks the joints. As a result, the tissue inside the joints, called synovium, starts to thicken and causes pain around the joints. The synovium is responsible for creating a fluid that lubricates the joints to help them move. Approximately 1.5 million people in the United States have Rheumatoid Arthritis. Women are almost three times as likely to have RA compared to men, and it’s disease usually begins between the ages of 30 and 60. People who have a genetic history of RA are more likely to develop the disease.
Symptoms of RA may include the following sensations in the joints: pain, tenderness, swelling, redness, warmth, stiffness, and loss of range. Swollen joints are a very common symptom for those with the disease. At times, it may be minimal, but it may also be very apparent. Another typical symptom is joint stiffness. Doctors will often use the direction of morning stiffness to measure the severity of a patient’s joint inflammation. Other RA symptoms include limping, anemia, fever, and fatigue.
To diagnose RA, your podiatrist will typically request x-rays to see how much damage there is in the joints. Blood tests may also be performed to show if there are any signs of anemia, or antibodies such as the rheumatoid factor. If you have previously been diagnosed with RA, you should know the disease may spread to your feet and ankles.
There are many non-surgical options that can be used to treat this ailment. Some of these options include physical therapy, foot massages, orthotics, bracing, supportive shoes, and steroid injections. Physical therapy is useful because it will help stretch and strengthen the joints in both the foot and ankle to improve joint function. Massages can help improve blood circulation which will be good for the feet. Choosing proper footwear will allow you to walk with comfortability if you are a sufferer from RA. Lastly, bracing will help stabilize the foot joints, limit deformities and decrease pain.
In severe cases, surgery may be a treatment option that should be considered. For those who cannot walk without experiencing pain and those whose deformities can not be managed with braces, surgery should be considered. Your podiatrist will recommend surgery if he or she believes it will improve your foot biomechanics.
Causes and Prevention Tips for Cracked Heels

Rough and cracked heels can cause discomfort and embarrassment. This can be a temporary condition as the causes and simple prevention tips are explored to achieve smooth, sandal-ready feet. Cracked heels can result from various factors, such as dry skin, lack of moisture, prolonged standing, and wearing open-back shoes. Additionally, certain medical conditions such as diabetes and thyroid issues may exacerbate the problem. Maintaining proper hydration is important in the prevention of cracked heels. This can be done by drinking plenty of water daily and keeping the feet moisturized. A good foot cream is best applied after a bath or shower. Exfoliate gently by regularly removing dead skin with a pumice stone or foot file to prevent buildup. It is beneficial to opt for supportive and well-fitting shoes to minimize pressure on your heels. The feet can be pampered with occasional warm foot baths while adding a few drops of essential oils for added relaxation. By following these simple tips, you can bid farewell to cracked heels and welcome the joy of smooth feet. If you would like more information about prevention techniques for cracked heels, it is suggested that you confer with a podiatrist.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact one of our podiatrists from Florida Ankle & Foot Institute. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our offices located in Tavernier, Marathon, and Key West, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.